Understanding Blood Clot in Foot Symptoms and Their Implications
Blood clots are more than just medical terms; they represent a crucial health issue that needs to be understood, especially when they occur in the foot. In this comprehensive article, we will delve deep into blood clot in foot symptoms, exploring their implications, potential risks, and essential preventive measures.
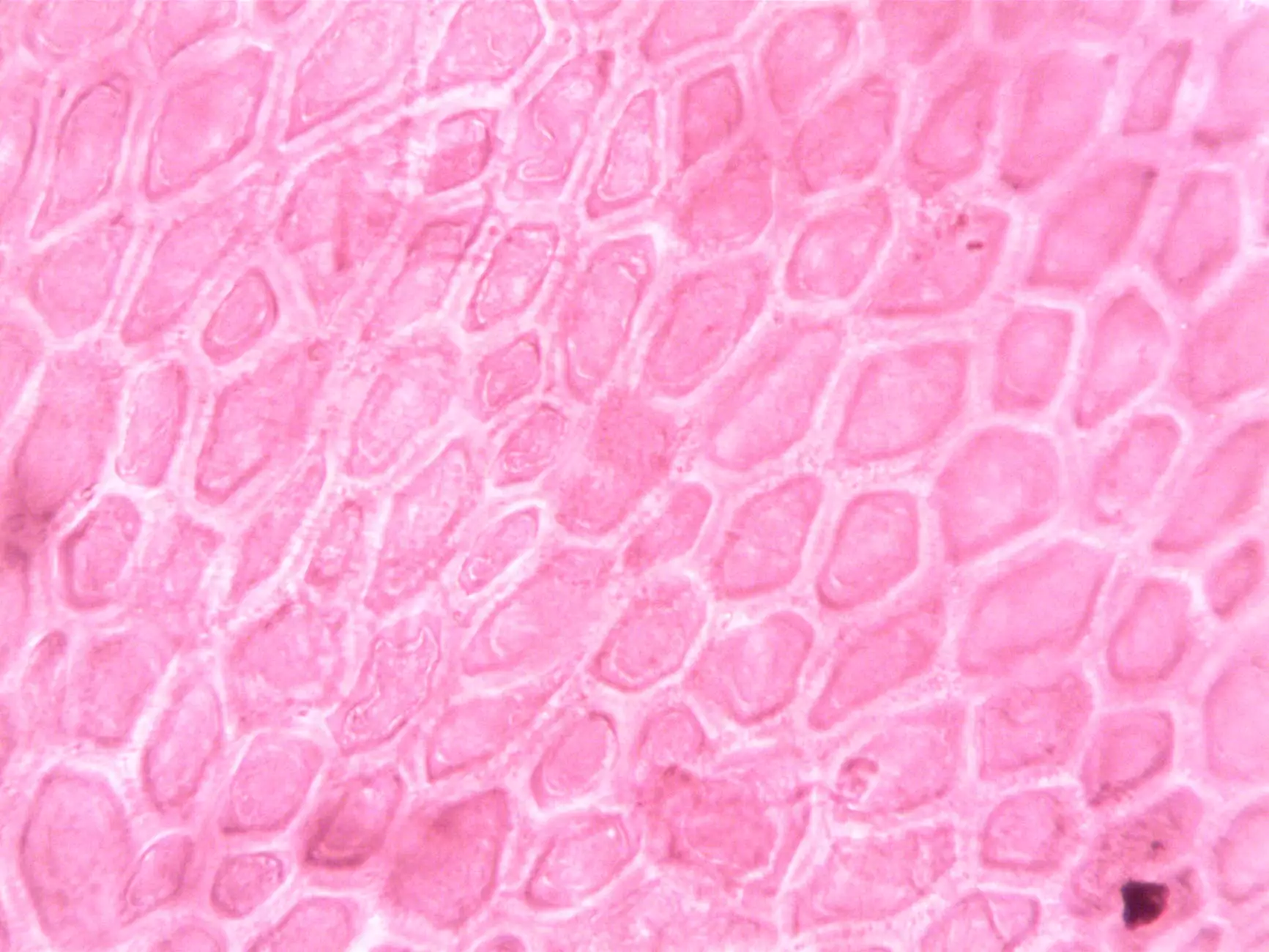
What is a Blood Clot?
A blood clot, or thrombus, is a gel-like mass formed from platelets and fibrin, aimed at stopping bleeding. While blood clots play a vital role in healing wounds, they can become dangerous when they form inappropriately, such as in the veins of the foot. Understanding when these clots form and recognizing the symptoms is essential for early intervention and treatment.
Types of Blood Clots
Blood clots can occur in various locations within the body, and their classifications primarily include:
- Deep Vein Thrombosis (DVT): Occurs when a blood clot forms in a deep vein, commonly in the legs or feet.
- Superficial Venous Thrombosis: A clot that forms in a vein close to the skin's surface.
- Pulmonary Embolism: A condition where a clot dislodges and travels to the lungs, which can be life-threatening.
Recognizing Blood Clot in Foot Symptoms
Identifying the symptoms of a blood clot in the foot is crucial for effective intervention. Here is a detailed list of blood clot in foot symptoms to watch for:
- Swelling: The affected foot may exhibit noticeable swelling, particularly in the ankle and calf area.
- Pain or Tenderness: A feeling of pain that may vary from a dull ache to sharp pain, often worsening when standing or walking.
- Changes in Skin Color: The skin over the affected area may appear red or discolored.
- Warmth: The clotted area may feel warmer to the touch compared to the surrounding skin.
- Pitting Edema: When pressing on the swollen foot, an indentation may remain, indicating fluid buildup.
Causes of Blood Clots in the Foot
Understanding the causes of blood clots helps in their prevention. Several risk factors contribute to the formation of clots:
- Prolonged Immobility: Sitting or lying down for extended periods, such as during long flights or bed rest.
- Injury: Damage to blood vessels from fractures, sprains, or surgical procedures can trigger clot formation.
- Medical Conditions: Certain illnesses, like cancer, heart disease, or hypercoagulable states, increase clot risk.
- Hormonal Factors: Use of hormonal contraceptives or hormone replacement therapy can elevate the risk.
- Obesity: Excess weight puts additional strain on the veins, increasing the likelihood of clot formation.
- Genetics: A family history of clotting disorders can predispose individuals to develop blood clots.
When to Seek Medical Attention
If you experience any symptoms suggestive of a blood clot in the foot, it is essential to act quickly. Immediate medical attention is necessary if you notice:
- A sudden increase in swelling
- Severe pain that is out of proportion to any injury
- Persistent warmth and discoloration
- Symptoms that coincide with shortness of breath or chest pain, as these can indicate a pulmonary embolism.
Diagnosis of Blood Clots
Diagnosing a blood clot usually involves several steps:
- Physical Examination: A healthcare provider will check for swelling, tenderness, and other symptoms.
- Ultrasound: This non-invasive test uses sound waves to create images of blood flow and detect clots.
- D-dimer Test: A blood test that measures clotting factors. High levels may suggest the presence of a clot.
- Computed Tomography (CT) or Magnetic Resonance Imaging (MRI): Imaging studies used to visualize blood clots in more complex cases.
Treatment Options for Blood Clots in the Foot
Treating a blood clot effectively can prevent serious health complications. The standard treatment approaches include:
- Blood Thinners: Medications such as heparin or warfarin are prescribed to prevent the clot from growing and reduce recurrence.
- Thrombolytics: In severe cases, these drugs dissolve large clots quickly.
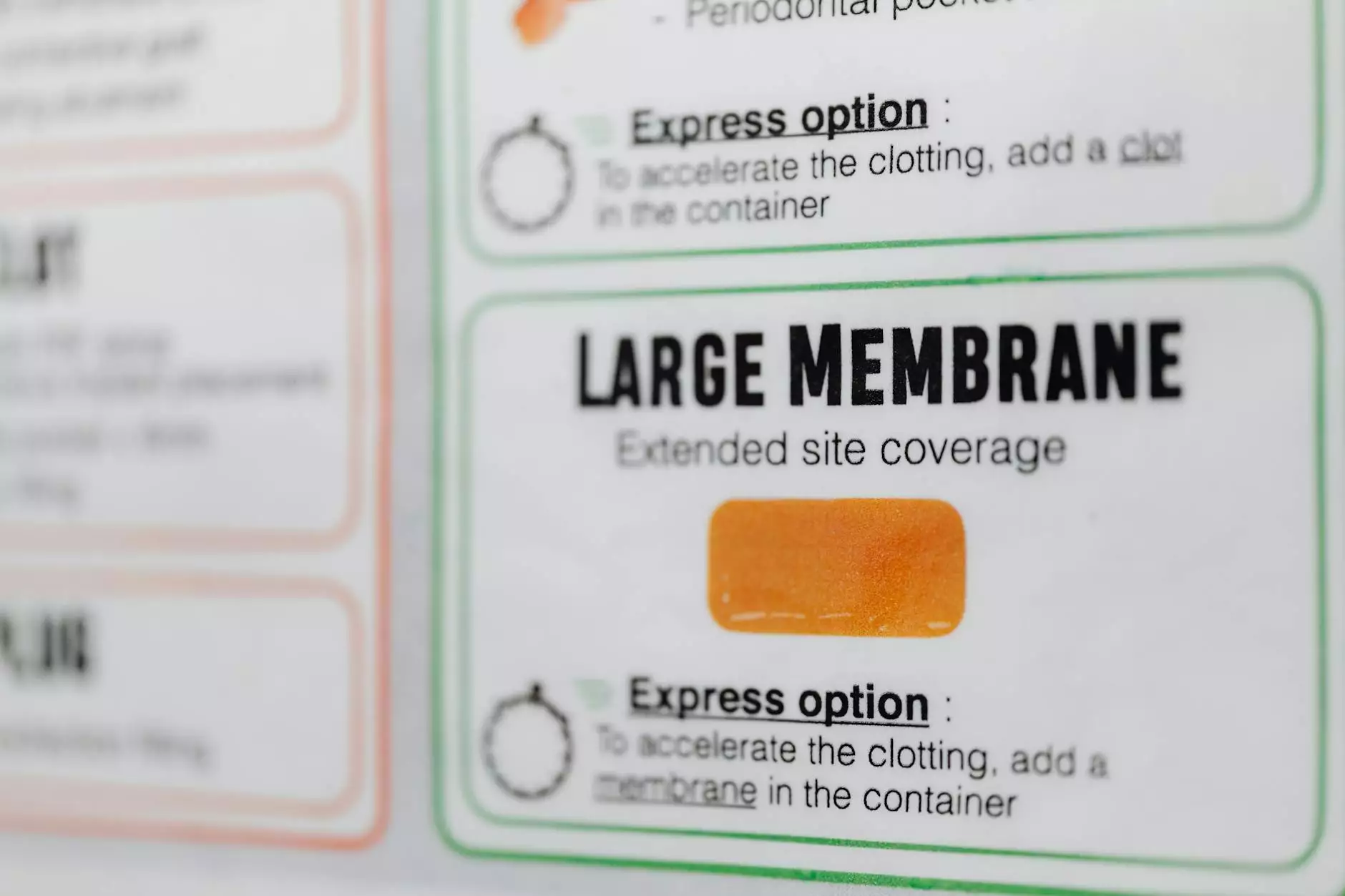
- Compression Therapy: Using compression stockings can help reduce swelling and assist blood flow in the legs.
- Catheter-Directed Thrombectomy: A minimally invasive procedure to remove large clots using a catheter.
- Surgery: In rare cases, surgical intervention may be necessary to remove a clot.
Preventing Blood Clots
Prevention is always better than cure. Below are crucial steps individuals can take to minimize the risk of blood clot formation:
- Stay Active: Regular physical activity promotes healthy circulation.
- Avoid Prolonged Immobility: Take breaks to stand, stretch, or walk during long periods of sitting.
- Maintain Healthy Weight: Adopting a balanced diet and regular exercise can help manage weight.
- Stay Hydrated: Adequate fluid intake can help prevent clotting.
- Follow Medical Advice: If you have risk factors or are in recovery from surgical procedures, always follow your healthcare provider's recommendations regarding mobility and medications.
Life After a Blood Clot: Recovery and Management
Experiencing a blood clot can be a life-altering event. Recovery and management strategies are crucial for long-term health:
- Regular Check-Ups: Follow-up with healthcare providers to monitor your condition.
- Medication Compliance: Adhere strictly to prescribed medications to prevent recurrence.
- Adopt a Healthy Lifestyle: Focus on a diet rich in fruits, vegetables, and whole grains and engage in regular exercise.
- Learn the Symptoms: Be vigilant about the symptoms of blood clots and remember what to watch out for.
Conclusion
Being informed about blood clot in foot symptoms, their causes, and preventative measures is a cornerstone of managing vascular health effectively. If you observe any concerning signs, seek immediate medical assistance. The interplay between awareness, lifestyle choices, and medical intervention plays a vital role in preventing serious complications associated with blood clots.
For further information and personalized advice, consult your healthcare provider or visit trufflesveinspecialists.com.